Abstract
Background: The National Comprehensive Cancer Network (NCCN) defines distress as an unpleasant emotional experience associated with the psychosocial complications of cancer. While distress is known to occur in 25-33% of patients with cancer, little is known about differences in distress across types of hematologic malignancies. Hodgkin lymphoma (HL) is a hematologic malignancy with a relatively good prognosis, where the goals of therapy are to cure patients and minimize the need for further treatment. First-line treatment includes combination chemotherapy and/or radiation, both of which are associated with an increased risk of late, therapy-related complications. We hypothesized that patients with HL suffer significant distress, and aimed to describe the severity and sources of distress among HL patients receiving active therapy vs. those who are long-term survivors.
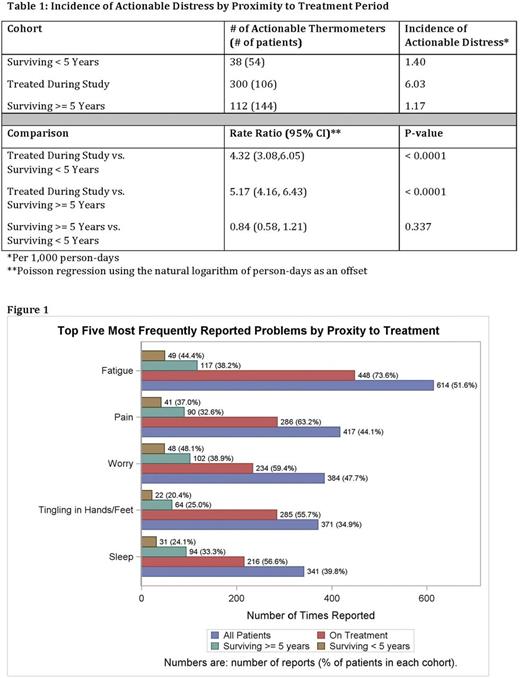
Methods: We performed a retrospective cohort study using electronic medical records. Eligible patients had pathologically confirmed HL and were seen in Duke Cancer Institute clinics between July 1, 2013 and November 16th, 2016. Patient-reported distress was assessed as part of routine care using the NCCN Distress Thermometer (DT). The DT includes an 11-point scale reflecting the overall distress level and an accompanying 39-item "problem list." Per the NCCN, a score of 4 or more signifies distress warranting clinical intervention (i.e., actionable distress). We abstracted data from the electronic medical record, including the DT score and accompanying "problem list" items, demographics, disease characteristics, and treatment regimens. Poisson regression was used to estimate the incidence of actionable distress.
Results: Data were abstracted for 304 patients with median age at diagnosis of 36 years, 56% Stage I/II disease, and 25% Early/Favorable prognosis. There were 106 (34.9%) receiving active treatment during the study period, 54 (17.8%) attending follow-up clinics after surviving less than 5 years, and 144 (47.4%) in follow-up for 5 or more years. DT data were available for 1,524 (72.2%) of the 2,110 clinical encounters for these patients. There was a median of 3 thermometers/patient (interquartile range [IQR]: 1-7, range: 1-47). Overall, distress scores were low (median DT=1, IQR: 0-4). Distress levels were similar with respect to proximity to active treatment, but the occurrence of actionable distress (>=4) was markedly different in these three patient groups; 450 (29.5%) of the 1,524 thermometers were actionable, with 300 (66.6%) of these from patients who were on active treatment, 38 (8.4%) from patients surviving < 5 years, and 112 (24.9%) from patients surviving >= 5 years. The incidence of actionable distress differed significantly between the cohorts (Table 1), with patients on treatment having an incidence rate more than 4 times that of either of the survivor cohorts. Fatigue, pain and worry were the three most frequently reported problems in all patients. However, we noted that these symptoms were more likely to be reported in patients on treatment than either of the survivor cohorts (Figure 1). Distinct differences were also observed in the survivor cohorts, with the short-term survivors being less likely to report symptom distress than those surviving 5 or more years. When separated by problem domain the majority of reported problems were physical (e.g., fatigue, pain; 60-70% in each cohort) and emotional (e.g., depression, worry; 20-25% in each cohort).
Conclusion:Patients receiving active therapy are at markedly increased risk of experiencing distress. Problems reported by HL patients represent primarily physical symptoms, but emotional problems represent a substantial proportion of the distress burden as well, even among long-term survivors Patterns of symptom distress suggest that those surviving beyond 5 years may face more frequent challenges compared with shorter-term survivors who recently completed therapy, although the types of issues faced by these survivor cohorts appear to be similar. Overall, patients on therapy experience more distress, yet distress occurs in long-term survivors as well. Although HL therapy aims to achieve a complete remission as quickly as possible while minimizing late effects, long-term attention to distress screening and management is needed regardless of outcomes, given the longer-term distress caused by physical symptoms and psychological concerns.
Troy: GamidaCell: Honoraria; The Emmes Corporation: Consultancy; The Community Data Roundtable: Consultancy. Feliciano: Seattle Genetics: Employment, Equity Ownership. Richhariya: Seattle Genetics: Employment, Equity Ownership. LeBlanc: Helsinn Therapeutics: Consultancy, Honoraria; Otsuka: Membership on an entity's Board of Directors or advisory committees; Cambia Health Foundation: Research Funding; AstraZeneca: Research Funding; Flatiron Health: Consultancy; Janssen: Honoraria; Seattle Genetics: Research Funding; Pfizer: Consultancy; Celgene: Honoraria; Boehringer Ingelheim: Membership on an entity's Board of Directors or advisory committees; American Cancer Society: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal